|
Nature Clinical Practice Endocrinology & Metabolism [Case Study] A Case of Hyponatremia Caused by Central Hypocortisolism
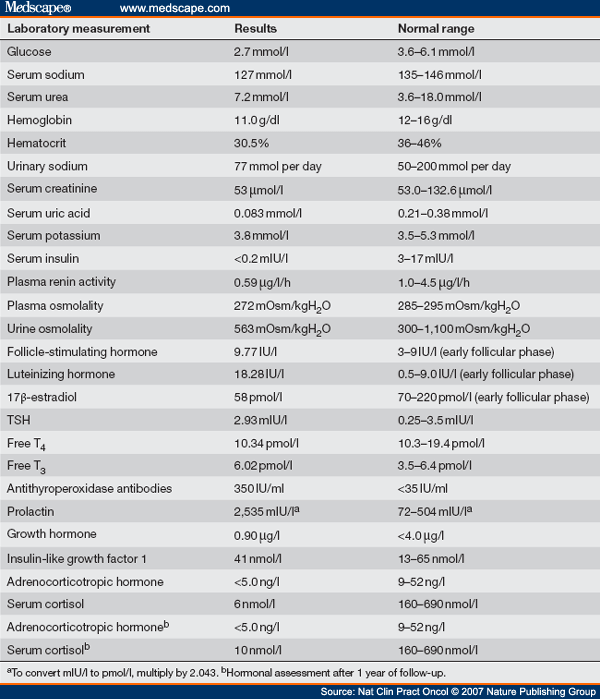
Gabriele Parenti; Valdo Ricca; Alessia Zogheri; Mario Serio; Massimo Mannelli; Alessandro Peri* Nat Clin Pract Endocrinol Metab. 2007;3(4):369-375.
In This Article
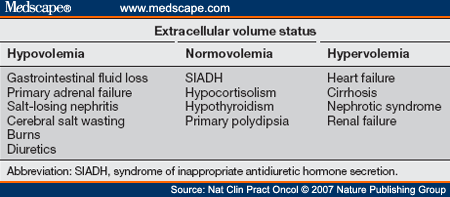
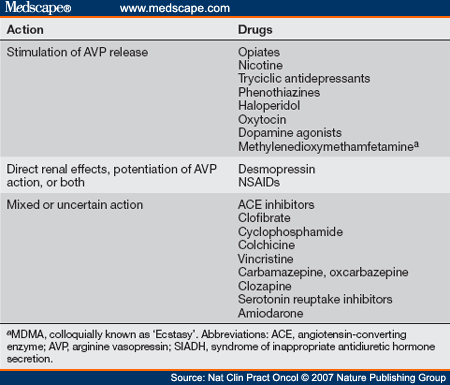
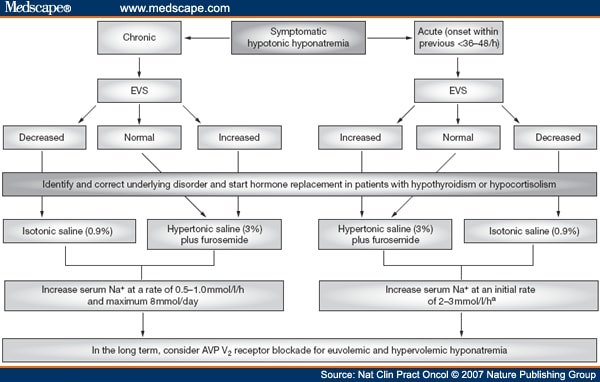
Treatment and Management As a general rule, the treatment of hyponatremia should be directed at the primary underlying disorder because such treatment might, in itself, correct the electrolyte imbalance. Thiazide diuretics and drugs that induce SIADH should be discontinued if possible, and hormone replacement therapy should be given to patients with suspected hypothyroidism or adrenal failure after hormonal evaluations have been performed. Determination of EVS represents the first step in the evaluation of hypotonic hyponatremia (Figure 2). If the extracellular volume is expanded, the underlying disease should be identified if not previously known, and specific treatment should be started. A scheme for the initial approach to treatment of symptomatic and asymptomatic hyponatremic patients is summarized in Figures 3 and 4.
Figure 2. Flowchart of the diagnostic work-up for hyponatremia. Abbreviations: EVS, extracellular volume status; SIADH, syndrome of inappropriate antidiuretic hormone secretion.
Figure 3. Schematic representation of the therapeutic approach for a patient with symptomatic hypotonic hyponatremia. aThe initial rate of sodium correction of 23 mmol/l/h should be reserved for severely symptomatic patients (i.e. those with seizures or coma). Abbreviations: AVP, arginine vasopressin; EVS, extracellular volume status.
Figure 4. Schematic representation of the therapeutic approach for a patient with asymptomatic hypotonic hyponatremia. Abbreviations: AVP, arginine vasopressin; EVS, extracellular volume status.
If hypovolemia is present, infusion of isotonic saline (0.9% NaCl) should be initiated, particularly in symptomatic patients, at an appropriate rate, to correct the estimated fluid and sodium deficit. Isotonic saline infusion is also appropriate for patients in whom it is initially difficult to distinguish between a hypovolemic and a euvolemic state, and this approach can also have diagnostic value—if euvolemic rather than hypovolemic hyponatremia is present, no improvement in serum sodium levels will be observed.[] If symptomatic, potentially life-threatening, euvolemic or hypervolemic hyponatremia is present, infusion of hypertonic saline (3% NaCl) should be considered. This approach, however, requires great caution, because severe side effects are possible (see below). Hypertonic saline is usually administered with furosemide (especially in hypervolemic patients), in order to limit expansion of the extracellular fluid volume that is induced by this treatment.[] Moreover, diuresis induced by furosemide is characterized by renal excretion of free water rather than sodium, which favors the correction of hyponatremia. A crucial point is the rate of correction of hypotonic hyponatremia. In chronic hyponatremia, a rapid increase in sodium levels puts the patient at risk for the development of cellular dehydration, and an extreme consequence might be central pontine myelinolysis (CPM). Most reported cases of CPM occurred after rates of correction higher than 12 mmol per day, but some cases have also occurred after correction rates of 9 mmol per day. Although other risk factors for CPM (such as malnutrition, hypokalemia or liver disease) were present in most of these cases,[] it is recommended not to exceed a correction rate of 8 mmol per day. An initial hourly rate of correction of 0.5-1.0 mmol/l is usually recommended. Nonetheless, in patients with acute (onset within the past 36-48 h) and severely symptomatic hyponatremia (i.e. with seizures or coma) a more rapid initial correction at an hourly rate of approximately 2-3 mmol/l is strongly recommended, because these patients have a high risk of morbidity and death.[] Infusion of hypertonic saline should be stopped when the patient becomes asymptomatic, levels of serum sodium reach 120 mmol/l, or both. A formula to calculate the rate of saline infusion can be of help in the management of these situations ( ).
Fluid restriction represents the safe mainstay of management of asymptomatic hypervolemic and euvolemic hyponatremia.[] In cases of SIADH, fluid restriction can be associated with a high-sodium diet (10 g per day orally). AVP V2 receptor blockade has been proposed as a promising alternative approach to treatment of euvolemic or hypervolemic hyponatremia. Selective V2-receptor antagonists promote free-water excretion and sodium and potassium reabsorption in the kidney, which normalizes serum sodium levels and prevents the hypokalemia associated with loop diuretics. Tolvaptan-a novel V2-receptor antagonist-seems to be more effective than fluid restriction for correction of euvolemic or hypervolemic hyponatremia, and does not cause an increase in adverse events.[] In this case hormonal replacement therapy with glucocorticoids represented the obvious therapeutic choice, and cortisone acetate was prescribed.
Next Section
Nat Clin Pract Endocrinol Metab. 2007;3(4):369-375. © 2007 Nature Publishing Group Cite this: [Case Study] A Case of Hyponatremia Caused by Central Hypocortisolism - Medscape - Apr 01, 2007.
Tables
Tables
Tables
Tables
Tables
Tables
References
Authors and Disclosures Authors and Disclosures Gabriele Parenti, Valdo Ricca, Alessia Zogheri, Mario Serio, Massimo Mannelli and Alessandro Peri*
Figure 2.
Figure 2.
Flowchart of the diagnostic work-up for hyponatremia. Abbreviations: EVS, extracellular volume status; SIADH, syndrome of inappropriate antidiuretic hormone secretion.
Figure 3.
Figure 3.
Schematic representation of the therapeutic approach for a patient with symptomatic hypotonic hyponatremia. aThe initial rate of sodium correction of 23 mmol/l/h should be reserved for severely symptomatic patients (i.e. those with seizures or coma). Abbreviations: AVP, arginine vasopressin; EVS, extracellular volume status.
Figure 4.
Figure 4.
Schematic representation of the therapeutic approach for a patient with asymptomatic hypotonic hyponatremia. Abbreviations: AVP, arginine vasopressin; EVS, extracellular volume status. (责任编辑:) |